Ezigulini eziningi ezinesifo sikashukela, inhliziyo iyathinteka. Ngakho-ke, cishe ama-50% abantu abahlaselwa yinhliziyo. Ngaphezu kwalokho, lezo zinkinga zingakhula ngisho nasebusheni.
Ukwehluleka kwenhliziyo kwisifo sikashukela kuhlotshaniswa nokuqukethwe okushukela okuphezulu emzimbeni, ngenxa yalokho i-cholesterol ifakwa ezindongeni ze-vascular. Lokhu kuholela ekunciphiseni kancane kwe-lumen yabo kanye nokuvela kwe-atherosulinosis.
Ngokuphikisana nesizinda se-atherossteosis, abanesifo sikashukela abaningi baba nesifo senhliziyo. Ngaphezu kwalokho, ngezinga elikhulayo le-glucose, ubuhlungu endaweni yesitho bubekezelelwa kakhulu. Futhi, ngenxa yokuqina kwegazi, amathuba we-thrombosis ayanda.
Ngaphezu kwalokho, abanesifo sikashukela bavame ukukhulisa umfutho wegazi, okufaka isandla ezinkingeni ngemuva kokuhlaselwa yisifo senhliziyo (aortic aneurysm). Esimweni sokuphinda senziwe kabusha kwesibalo sasemva kokufiswa, amathuba okuhlaselwa yinhliziyo okuphindaphindiwe noma nokufa empeleni kukhuphuka kakhulu. Ngakho-ke, kubaluleke kakhulu ukwazi ukuthi yimuphi umonakalo wenhliziyo osushukela nokuthi ungayelapha kanjani le nkinga.
Izimbangela zokuphazamiseka kwenhliziyo nezimpawu zobungozi
Isifo sikashukela sinesikhathi esifushane sokuphila ngenxa yezinga likashukela egazini eliphakeme njalo. Lesi simo sibizwa nge-hyperglycemia, esinomthelela oqondile ekwakhekeni kwezigcawu ze-atherosulinotic. Lokhu okugcina kuncane noma kuvimbele i-lumen yemikhumbi, okuholela ku-ischemia yemisipha yenhliziyo.
Iningi labodokotela liyaqiniseka ukuthi ukweqiwa ushukela kuphakamisa ukungasebenzi kahle kwendawo - indawo yokuqongelela i-lipid. Ngenxa yalokhu, izindonga zemikhumbi ziba zivumeleka ngokwengeziwe futhi zifakwa ezigcotsheni.
I-Hyperglycemia nayo inomthelela kusebenze kokucindezela kwe-oxidative kanye nokwenziwa kwama-free radicals, okubuye kube nomthelela omubi kwi-endothelium.
Ngemuva kochungechunge lwezifundo, kwasungulwa ubudlelwano phakathi kwamathuba okuba nesifo senhliziyo ku-mellitus yesifo sikashukela kanye nokwanda kwe-hemoglobin ye-glycated. Ngakho-ke, uma i-HbA1c inyuka nge-1%, khona-ke ingozi ye-ischemia inyuka ngo-10%.
Isifo sikashukela kanye nesifo senhliziyo sizoba imiqondo ehambisanayo uma isiguli sivezwa yizinto ezingezinhle:
- ukukhuluphala
- uma esinye sezihlobo sikashukela sinokuhlaselwa yisifo senhliziyo;
- imvamisa yegazi;
- ukubhema;
- ukusetshenziswa kabi kotshwala;
- ukuba khona kwe-cholesterol ne-triglycerides egazini.
Iziphi izifo zenhliziyo ezingaba yinkinga yesifo sikashukela?
 Imvamisa, nge-hyperglycemia, isifo sikashukela senhliziyo sikhula. Lesi sifo sivela lapho ukungasebenzi kahle kwe-myocardium ezigulini kunxephezela ukunxeshezelwa kashukela.
Imvamisa, nge-hyperglycemia, isifo sikashukela senhliziyo sikhula. Lesi sifo sivela lapho ukungasebenzi kahle kwe-myocardium ezigulini kunxephezela ukunxeshezelwa kashukela.
Imvamisa lesi sifo sicishe sibe njenge-asymptomatic. Kepha kwesinye isikhathi isiguli sihlushwa izinhlungu ezihlukumezayo kanye nokushaya kwenhliziyo okuguquguqukayo (tachycardia, bradycardia).
Ngasikhathi sinye, isitho esiyinhloko siyayeka ukupompa igazi futhi sisebenze ngemodi ebanzi, ngenxa yokuthi ubukhulu bayo bukhuphuka. Ngakho-ke, lesi simo sibizwa ngokuthi yinhliziyo yesifo sikashukela. I-Pathology ekukhuleni ingabonakaliswa ngobuhlungu obuzulazulayo, ukuvuvukala, ukuphefumula nokuphefumula kwesifuba okwenzeka ngemuva kokuzivocavoca.
Isifo senhliziyo esinesifo sikashukela sikhula kaningi kathathu kunabantu abaphilile. Kuyaphawuleka ukuthi ubungozi besifo senhliziyo ayihambelani nobunzima besifo esikhona, kepha isikhathi saso.
I-Ischemia in diabetesics ihlala iqhubeka ngaphandle kwezimpawu eziphinyisiwe, okuvame ukuholela ekwakhiweni kwe-infarction yemisipha yenhliziyo engenabuhlungu. Ngaphezu kwalokho, lesi sifo siqhubeka ngamagagasi, lapho ukuhlaselwa kanzima kuthathelwa indawo inkambo engapheli.
Izici zesifo senhliziyo ezi-coronary ukuthi ngemuva kokushayeka kwenhliziyo ku-myocardium, ngokumelene nesizinda se-hyperglycemia, i-cardiac syndrome, ukuhluleka kwenhliziyo, kanye nomonakalo wemithambo yegazi eqala ukukhula ngokushesha. Isithombe somtholampilo se-ischemia in sikashukela:
- ukuphefumula
- arrhythmia;
- ubunzima bokuphefumula
- ukucindezela kwezinhlungu enhliziyweni;
- ukukhathazeka okuhambisana nokwesaba ukufa.
Ukuhlanganiswa kwe-ischemia nesifo sikashukela kungaholela ekwakhiweni kwe-myocardial infarction. Ngaphezu kwalokho, le nkinga inezici ezithile, njengokubetha kwenhliziyo okuphazamisekile, i-edema yamaphaphu, izinhlungu zenhliziyo ezikhanyayo kwikholarbone, intamo, umhlathi noma ihlombe lehlombe. Kwesinye isikhathi isiguli sihlangabezana nobuhlungu obukhulu obucindezelekayo esifubeni, isicanucanu kanye nokuhlanza.
Ngeshwa, iziguli eziningi zihlaselwa yisifo senhliziyo ngoba aziqapheli nesifo sikashukela. Okwamanje, ukuchayeka kwi-hyperglycemia kuholela ezinkingeni ezibulalayo.
Ngo diabetesics, amathuba okuthuthukisa angina pectoris kabili. Ukuvezwa kwayo okuyinhloko ama-palpitations, i-malaise, ukujuluka kanye nokuphefumula komoya.
I-Angina pectoris, eyavela ngemuva kwesifo sikashukela, inezimpawu zayo. Ngakho-ke, ukukhula kwayo akuthinteki ngobunzima besifo esikhona, kepha isikhathi sesifo senhliziyo. Ngaphezu kwalokho, ezigulini ezinoshukela omningi, ukunikezwa kwegazi okunganele kuma-myocardium kukhula ngokushesha okukhulu kunakubantu abanempilo.
Ema-diabetes amaningi, izimpawu ze-angina pectoris zimnene noma azikho ngokuphelele. Ngaphezu kwalokho, zivame ukuba nokungasebenzi kahle kusigqi senhliziyo, esivame ukuphela ekufeni.
Omunye umphumela wesifo sikashukela sohlobo 2 ukwehluleka kwenhliziyo, okufana nezinye izinkinga zenhliziyo ezivela ku-hyperglycemia, futhi kunemininingwane yayo. Ngakho-ke, ukwehluleka kwenhliziyo ngoshukela ophezulu kuvame ukukhula esemncane, ikakhulukazi emadodeni. Izimpawu zokuphawulwa kwalesi sifo zibandakanya:
- ukuvuvukala nokuqhakaza kwemilenze;
- ukunwetshwa kwenhliziyo ngosayizi;
- ukuchama njalo
- ukukhathala;
- ukukhuphuka kwesisindo somzimba, okuchazwa ngokugcinwa kwamanzi emzimbeni;
- Isiyezi
- ukuphefumula
- ukukhwehlela.
I-Diabetesic myocardial dystrophy nayo iholela ekuphulweni kwesigqi sokushaya kwenhliziyo. I-Pathology yenzeka ngenxa yokungasebenzi kahle kwezinqubo ze-metabolic, icasulwa ukuntuleka kwe-insulin, okuyinkimbinkimbi yokudlula kwe-glucose ngokusebenzisa amaseli e-myocardial. Ngenxa yalokhu, ama-acid anama-oxidised anqwabelana emisipha yenhliziyo.
Inkambo ye-myocardial dystrophy iholela ekubukekeni kwe-factor ye-conduction ukuphazamiseka, i-fhningering arrhythmias, i-extrasystoles noma i-parasystoles. Futhi, i-microangiopathy kushukela sinomthelela ekunqotshweni kwemikhumbi emincane eyondla i-myocardium.
I-sinus tachycardia yenzeka ngokweqile kwemizwa noma ngokomzimba. Ngemuva kwakho konke, ukusebenza kwenhliziyo okusheshayo kuyadingeka ukuhlinzeka umzimba ngezakhi zomsoco nomoya-mpilo. Kepha uma ushukela wegazi ukhuphuka njalo, khona-ke inhliziyo iyaphoqwa ukuba isebenze ngemodi ethuthukisiwe.
Kodwa-ke, kuma-diabetes, i-myocardium ayikwazi ukungena ngokushesha. Ngenxa yalokhu, umoya-mpilo nezakhi zomsoco akungeni enhliziyweni, okuvame ukuholela ekuhlaselweni yinhliziyo nokufa.
Nge-neuropathy yesifo sikashukela, ukushintshashintsha kwesilinganiso senhliziyo kungakhula. Ngokwesimo esinjalo somlingiswa, i-arrhythmia yenzeka ngenxa yokushintshashintsha kokumelana kohlelo lwe-peripheral vascular system, okumele lwenziwe yi-NS.
Enye inkinga yesifo sikashukela yi-orthostatic hypotension. Baboniswa ngokuncipha kwengcindezi yegazi. Izimpawu ze-hypertension yizisiyezi, i-malaise, ne-failing. Ubuye abonakale nobuthakathaka ngemuva kokuvuka nekhanda elihlala likhona.
Njengoba ngokunyuka okungapheli koshukela wegazi kunezinkinga eziningi, kubalulekile ukwazi ukuthi ungayiqinisa kanjani inhliziyo kushukela nokuthi yikuphi ukwelashwa ongakukhetha uma lesi sifo sesivele sivele.
Ukwelashwa kwezidakamizwa zezifo zenhliziyo ezinesifo sikashukela
 Isisekelo sokwelashwa ukuvimbela ukukhula kwemiphumela okungenzeka futhi kumise ukuqhubeka kwezinkinga ezikhona. Ukuze wenze lokhu, kubalulekile ukwenze i-glycemia yokuzijwayeza, ukulawula amazinga kashukela futhi ivikele ukuthi ingakhuphuki ngisho namahora ama-2 ngemuva kokudla.
Isisekelo sokwelashwa ukuvimbela ukukhula kwemiphumela okungenzeka futhi kumise ukuqhubeka kwezinkinga ezikhona. Ukuze wenze lokhu, kubalulekile ukwenze i-glycemia yokuzijwayeza, ukulawula amazinga kashukela futhi ivikele ukuthi ingakhuphuki ngisho namahora ama-2 ngemuva kokudla.
Ngale njongo, ngesifo sikashukela sohlobo 2, ama-ejenti eqenjini le-Biguanide anqunyelwe. Lezi yiMetformin neSiofor.
Umphumela weMetformin unqunywa amandla ayo okuvimbela i-gluconeogeneis, kusebenze i-glycolysis, ethuthukisa ukugcinwa kwe-pyruvate ne-lactate emisipha yemisipha namafutha. Futhi, umuthi uvimbela ukukhula kokukhula kwemisipha ebushelelezi yezindonga zemithambo futhi kuthinta inhliziyo kahle.
Umthamo wokuqala ngu-100 mg ngosuku. Kodwa-ke, kunezindlela eziningi zokuphambana ekuphuzeni umuthi, ikakhulukazi ukuba uqaphele kulabo abanokulimala kwesibindi.
Futhi, ngesifo sikashukela sohlobo 2, iSiofor imvama ukunqunywa, esebenza ngempumelelo ikakhulukazi lapho ukudla nokuvivinya umzimba kunganikeli ekunciphiseni isisindo. Umthamo wansuku zonke ukhethwa ngokuhlukile ngokuya nge-glucose.
Ukuze iSiofor isebenze, inani layo livinjelwa njalo - lisuka kumathebulethi ayi-1 kuye kwayi-3. Kepha umthamo omkhulu wesidakamizwa kufanele ungabi ngaphezu kwama-gramu amathathu.
I-Siofor i-contraindicated uma kwenzeka kunesifo sikashukela esincike ku-insulin, infarction ye-myocardial, ukukhulelwa, ukwehluleka kwenhliziyo nezifo zamaphaphu ezinzima. Futhi, umuthi awuthathwa uma isibindi, izinso futhi sisesimweni sokukhubazeka sikashukela kusebenza kahle. Ngaphezu kwalokho, uSiofor akufanele adakwe uma izingane noma iziguli ezingaphezu kuka-65 ziphathwa.
Ukususa i-angina pectoris, ischemia, ukuvimbela ukukhula kwe-myocardial infarction kanye nezinye izinkinga zenhliziyo ezivela kwisifo sikashukela, kubalulekile ukuthatha amaqembu ahlukahlukene wezidakamizwa:
- Izidakamizwa ze-antihypertensive.
- Ama-ARB - ukuvimbela i-myocardial hypertrophy.
- I-Beta-blockers - yenza izinga lokushaya kwenhliziyo libe njalo futhi lijwayeze umfutho wegazi.
- I-diuretics - yehlisa ukuvuvukala.
- AmaNitrate - yeka ukushaya kwenhliziyo.
- Ama-inhibitors e-ACE - abe nomthelela ojwayelekile wokuqinisa enhliziyweni;
- Ama-anticoagulants - enza igazi lingabonakali kangako.
- Ama-glycosides akhonjiswa i-edema ne-atrial fibrillation.
Ngokukhuphuka, ngesifo sikashukela sohlobo 2, esihambisana nezinkinga zenhliziyo, udokotela obonayo unquma uDibicor. Isebenza izinqubo ze-metabolic ezicutshini, zibanikeze amandla.
I-Dibicor ithinta kahle isibindi, inhliziyo nemithambo yegazi. Ngaphezu kwalokho, ngemuva kwezinsuku eziyi-14 kusukela kuqale lo muthi, kukhona ukwehla kokuhlushwa ushukela wegazi.
Ukwelashwa ngokuhluleka kwenhliziyo kuqukethe ukuthatha amaphilisi (250-500 mg) 2 p. ngosuku. Ngaphezu kwalokho, i-Dibikor inconywa ukuphuza ngemizuzu engama-20. ngaphambi kokudla. Inani eliphezulu lomthamo wansuku zonke wezidakamizwa ngu-3000 mg.
I-Dibicor is contraindicated ebuntwaneni ngesikhathi sokukhulelwa, i-lactation futhi uma kwenzeka ukungabekezelelani kwe-taurine. Ngaphezu kwalokho, i-Dibicor ayikwazi ukuthathwa nge-glycosides ye-cardiac ne-BKK.
Izindlela zokwelapha
Abaningi besifo sikashukela banendaba nokuthi bangelapha kanjani ukwehluleka kwenhliziyo ngokuhlinzwa. Ukwelashwa nge-radical kwenziwa lapho kuqiniswa uhlelo lwezinhliziyo ngosizo lwezidakamizwa akuzange kulethe imiphumela oyifunayo. Izinkomba zezinqubo zokuhlinzwa yilezi:
- izinguquko ku-cardiogram;
- uma indawo yesifuba ihlala ibuhlungu;
- ukuvuvukala
- arrhythmia;
- ukusolwa kwenhliziyo okusolisayo;
- i-angina pectoris ethuthukayo.
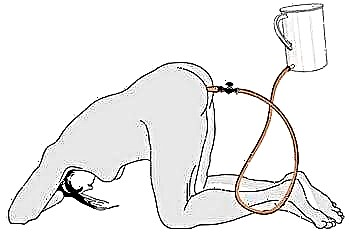
Ukuhlinzwa kwezehluleki zenhliziyo kufaka i-balodon vasodilation. Ngosizo lwayo, ukuncipha komthambo, ondla inhliziyo, kuyaqedwa. Ngesikhathi senqubo, kufakwa i-catheter emthanjeni, okulethwe kuyo ibhaluni endaweni yenkinga.
I-storing ye-aortocoronary imvamisa yenziwa lapho kufakwa isakhiwo se-mesh emthanjeni ovimbela ukwakheka kwama-cholesterol plaques. Futhi nge-coronary artery bypass grafting kudala izimo ezengeziwe zokugeleza kwegazi kwamahhala, okunciphisa kakhulu ingozi yokuphindelela.
Uma kwenzeka isifo se-cardiodystrophy sikashukela, kukhombisa ukwelashwa okuhlinzwa ngokufakwa ngaphakathi kwe-pacemaker. Le divayisi ithwebula noma yiziphi izinguquko enhliziyweni bese ziyazilungisa ngaso leso sikhathi, ezinciphisa amathuba okuba nama-arrhythmias.
Kodwa-ke, ngaphambi kokwenza lokhu kusebenza, kubalulekile ukuthi ungagcini ngokujwayeza ukugcwala kweglucose, kepha futhi nokunciphisela ushukela. Njengoba nokungenelela okuncane (ngokwesibonelo, ukuvula i-abscess, ukususwa kwezipikili), okwenziwa ekwelashweni kwabantu abanempilo ngesisekelo sokuphuma, kwabanesifo sikashukela kwenziwa esibhedlela sokuhlinzwa.
Ngaphezu kwalokho, ngaphambi kokungenelela okukhulu kokuhlinzwa, iziguli ezine-hyperglycemia zidluliselwa kwi-insulin. Kulokhu, kwethulwa i-insulin elula (imithamo engu-3-5). Futhi phakathi nosuku kubalulekile ukulawula i-glycosuria noshukela wegazi.
Njengoba isifo senhliziyo nesifo sikashukela kuyimiqondo ehambisanayo, abantu abane-glycemia badinga ukubheka njalo ukusebenza kohlelo lwethambo nenhliziyo. Kubalulekile futhi ukulawula ukuthi ushukela wegazi ukhuphuke kangakanani, ngoba nge-hyperglycemia enzima, ukuhlaselwa yinhliziyo kungenzeka, okuholela ekufeni.
Kwividiyo ekulesi sihloko, isihloko sesiifo senhliziyo sikashukela siyaqhubeka.